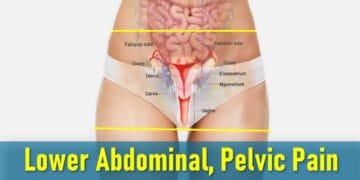
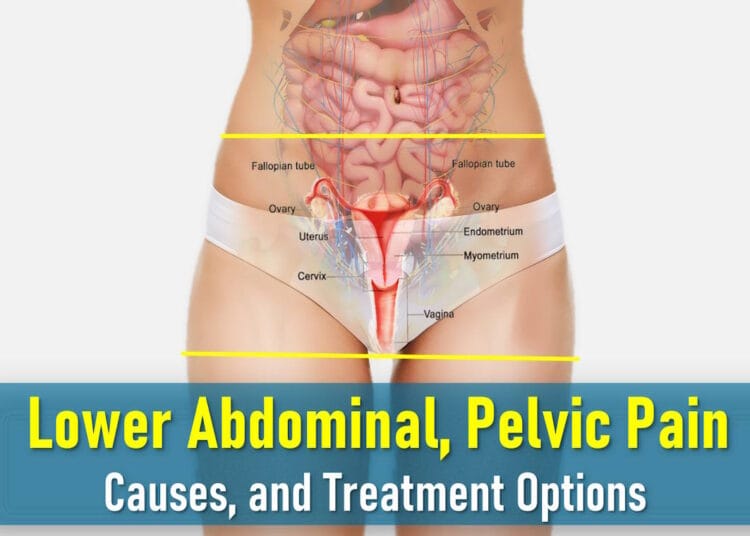
Pelvic pain refers to discomfort in the lower abdomen, which can range from mild to severe. It may be constant or intermittent, sharp and localized, or a dull ache spread across the pelvic region. For some, the pain is severe enough to disrupt daily life. Women often experience pelvic pain during menstruation or sexual activity, while men may notice it due to prostate issues. In both genders, infections, urinary tract problems, muscle or bone conditions, or intestinal issues can also trigger pelvic discomfort. Many women deal with multiple causes simultaneously.
Diagnosing pelvic pain typically involves lab tests, imaging, or other medical evaluations. Treatment depends on the underlying cause, pain intensity, and frequency.
What Is Pelvic Pain?
Pelvic pain originates from organs in the lowest part of the abdomen, including the uterus, ovaries, fallopian tubes, bladder, or bowel. Sometimes, the pain stems from nearby bones, muscles, nerves, or joints, making it a complex issue with many possible causes. Women are more likely than men to experience pelvic pain, and it can be classified as:
- Acute pelvic pain: A sudden, first-time occurrence.
- Chronic pelvic pain: Persistent discomfort lasting more than six months.
Common Symptoms of Pelvic Pain in Women
Pelvic pain often presents alongside other symptoms, depending on the affected area:
Bowel-Related Pain
Discomfort may come and go, varying in intensity and duration. Many describe it as cramping or colic, often relieved after a bowel movement. Additional symptoms include:
- Bloating or abdominal swelling
- Excessive gas
- Alternating diarrhea and constipation (common in irritable bowel syndrome)
Bladder-Related Pain
Painful bladder syndrome involves persistent discomfort or pressure in the pelvic area, fluctuating in severity. Symptoms often include:
- Frequent urination
- Pain while urinating
- Reduced bladder control
These symptoms typically persist for over six weeks without an infection as the cause.
Pain During Sex (Dyspareunia)
Pelvic pain during or after intercourse is called dyspareunia and is categorized as:
- Superficial pain: Felt at the genital opening.
- Deep pain: Occurs deeper in the pelvis, often linked to conditions like endometriosis, ovarian cysts, or pelvic inflammatory disease.
While some women experience both types, most have one predominant form.
Causes of Pelvic Pain in Women
Pelvic pain in women can stem from various conditions, ranging from normal bodily functions to serious medical issues. Understanding these causes can help identify potential triggers and guide treatment.
Ovulation Pain (Mittelschmerz)
During ovulation, the release of an egg from the ovary can cause sharp, sudden pain known as Mittelschmerz (German for “middle pain,” as it occurs mid-cycle). The discomfort typically lasts a few hours but may be severe for some women. The pain can switch sides each month, depending on which ovary releases the egg.
You can try our Ovulation Calculator to know your most likely ovulation date.
Menstrual Cramps (Dysmenorrhea)
Most women experience mild cramping during their periods, but for about 1 in 10, the pain is severe enough to disrupt daily life, sometimes making work or school difficult. This intense menstrual pain, called dysmenorrhea, results from uterine contractions as the uterus sheds its lining.
Pelvic Inflammatory Disease (PID)
PID is a bacterial infection of the pelvic organs, often caused by sexually transmitted infections like chlamydia or gonorrhea. Symptoms include:
- Lower abdominal or pelvic pain
- Fever
- Abnormal vaginal discharge or bleeding
Without treatment, PID can lead to long-term complications, including infertility.
Ovarian Cysts: Rupture or Torsion
Ovarian cysts, fluid-filled sacs on the ovaries, are usually harmless. However, if a cyst ruptures or twists (torsion), it can cause sudden, severe pain. While many cysts resolve on their own, persistent symptoms may require medical attention.
Fibroid Degeneration
Uterine fibroids are noncancerous growths that often cause no symptoms. However, if a fibroid outgrows its blood supply, it can shrink (degenerate), leading to sharp, localized pain. Other fibroid symptoms include heavy periods, bloating, and frequent urination.
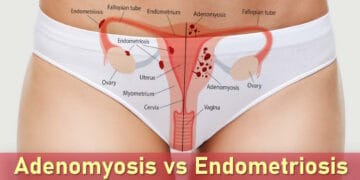
Endometriosis
Endometriosis occurs when uterine-like tissue grows outside the womb, often on the ovaries, fallopian tubes, or pelvic lining. Common in women aged 13–50 (especially those struggling with infertility), it causes:
- Severe period pain
- Pain during sex (deep pelvic pain)
- Chronic lower abdominal discomfort
Chronic Pelvic Pain
When pelvic pain persists for six months or longer without a clear cause, it’s classified as chronic. Contributing factors may include:
- Undiagnosed conditions (e.g., endometriosis, adhesions)
- Psychological stress or a history of trauma
- Muscular or nerve dysfunction
Treatment focuses on pain management, sometimes incorporating physical therapy or counseling.
Appendicitis
Though not exclusive to women, appendicitis, inflammation of the appendix, can cause escalating lower right abdominal pain, nausea, and vomiting. Immediate surgery is often needed to prevent a ruptured appendix, which can be life-threatening.
Irritable Bowel Syndrome (IBS)
IBS is a common digestive disorder that affects the large intestine. While the exact cause remains unknown, symptoms often include:
- Abdominal cramping or pain (often relieved by bowel movements)
- Bloating and gas
- Alternating diarrhea and constipation
Though there’s no cure for IBS, dietary changes, stress management, and medications can help manage symptoms effectively.
Urinary Tract Infections (Cystitis)
Bladder infections are particularly common in women due to their shorter urethra. Symptoms typically include:
- Burning sensation during urination
- Frequent urge to urinate
- Lower abdominal or pelvic discomfort
While most UTIs clear quickly with antibiotics, some cases may develop into interstitial cystitis (painful bladder syndrome), a chronic condition causing persistent pelvic pain without evidence of infection.
Post-Surgical Adhesions
After abdominal or pelvic surgery, internal scar tissue can form abnormal connections between organs. These adhesions most commonly affect the bowel and may cause:
- Chronic pelvic pain
- Digestive disturbances
- Pain during movement or sexual activity
Strangulated Hernia
When abdominal muscles weaken, internal tissues can protrude, creating a noticeable bulge. If the herniated intestine becomes trapped and loses blood supply (strangulation), symptoms become severe:
- Sudden, intense pain in the affected area
- Nausea and vomiting
- Redness or discoloration at the hernia site
This constitutes a medical emergency requiring immediate attention.
Musculoskeletal Issues
Problems with bones, joints, or muscles in the pelvic region can manifest as pelvic pain. Common sources include:
- Lower back problems
- Hip joint disorders
- Pelvic floor muscle dysfunction
The pain may be difficult to localize, sometimes feeling like generalized pelvic discomfort.
Sexually Transmitted Infections (STIs)
Various STIs can cause pelvic pain and other symptoms:
- Unusual vaginal discharge
- Pain during intercourse or urination
- Genital sores or rashes
- Abnormal bleeding between periods
Regular STI testing and safe sex practices are crucial for prevention and early treatment.
Pelvic Pain During Pregnancy
Pregnancy-related pelvic pain can range from normal discomfort to signs of serious complications. Understanding these differences helps expectant mothers know when to seek medical attention.
Miscarriage
Miscarriage refers to pregnancy loss before 24 weeks, with most occurring in the first trimester. Warning signs include:
- Vaginal bleeding (often with clots)
- Lower abdominal or pelvic cramping
- Passage of tissue from the vagina
Ectopic Pregnancy
This life-threatening condition occurs when a fertilized egg implants outside the uterus, usually in a fallopian tube. Symptoms demand immediate medical attention:
- Sharp or gradually worsening pain on one side of the pelvis
- Dark vaginal bleeding (may differ from normal period flow)
- Shoulder tip pain (indicates internal bleeding)
Ruptured Corpus Luteum Cyst
The corpus luteum, a hormone-producing structure formed after ovulation, sometimes develops into a cyst. While usually harmless, rupture can cause:
- Sudden, sharp pelvic pain (typically in first trimester)
- One-sided discomfort
- Possible light spotting
Preterm Labor
Labor beginning before 37 weeks requires prompt medical intervention. Warning signs include:
- Regular, rhythmic pelvic contractions
- Pelvic pressure or backache
- Vaginal fluid leakage (water breaking)
- Bloody mucus discharge (“show”)
Placental Abruption
This rare but serious condition occurs when the placenta separates prematurely from the uterine wall. Symptoms include:
- Sudden, severe abdominal/pelvic pain
- Firm, tender uterus
- Vaginal bleeding (may be concealed)
- Decreased fetal movement
Diagnosing Pelvic Pain
Pelvic pain can have various causes, ranging from mild to potentially life-threatening. To accurately diagnose the condition, healthcare providers follow a structured approach that includes clinical evaluation, diagnostic tests, and, if needed, specialized procedures.
Initial Evaluation
- Medical History: Your provider will ask detailed questions about the nature, location, timing, and intensity of your pain, as well as any related symptoms such as bleeding, discharge, or urinary issues.
- Physical Examination: A thorough physical exam—including a pelvic exam—is performed to check for tenderness, swelling, masses, or anatomical abnormalities.
Common Diagnostic Tests
1. Laboratory Tests
- Urinalysis: To detect urinary tract infections or hematuria (blood in urine).
- Vaginal and Cervical Swabs: Used to test for sexually transmitted infections (STIs) such as chlamydia, gonorrhea, and trichomoniasis.
- Pregnancy Test: To rule out or confirm pregnancy-related conditions, including ectopic pregnancy.
2. Imaging Studies
- Pelvic Ultrasound: The first-line imaging technique used to evaluate the uterus, ovaries, and other pelvic organs for conditions like ovarian cysts, fibroids, or early pregnancy complications.
- Transvaginal Ultrasound: Provides a more detailed view of pelvic structures and is especially useful in early pregnancy or when endometriosis or pelvic inflammatory disease is suspected.
- Emergency Ultrasound: Essential if there is concern for ectopic pregnancy, miscarriage, or other urgent conditions.
3. Specialized Procedures
- Laparoscopy: A minimally invasive surgical procedure that uses a camera inserted through a small incision in the abdomen. It is often used to diagnose endometriosis, adhesions, or unexplained pelvic pain when other tests are inconclusive.
- Colonoscopy or Gastroscopy: These may be recommended if gastrointestinal causes are suspected, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or diverticulitis.
Treatment and Management of Pelvic Pain
Effective treatment depends on identifying the root cause of the pain. Options range from conservative measures to medical or surgical interventions.
Self-Care and Conservative Treatments
- Over-the-Counter Pain Relief: Medications like acetaminophen or ibuprofen can help relieve mild to moderate pain, especially menstrual cramps or muscle-related discomfort.
- Heat Therapy: Applying a heating pad to the lower abdomen can soothe muscle spasms and reduce cramping.
- Pelvic Floor Exercises: Kegel exercises and physical therapy may help manage chronic pelvic pain associated with muscle dysfunction or pelvic floor disorders.
- Lifestyle Adjustments: Stress management, regular physical activity, and dietary modifications may alleviate symptoms, especially in cases of IBS or chronic pelvic pain syndrome.
Medical and Surgical Treatments
- Antibiotics: Prescribed for infections such as pelvic inflammatory disease (PID) or urinary tract infections (UTIs).
- Hormonal Therapy: Birth control pills or hormone treatments may be used for conditions like endometriosis or menstrual-related pain.
- Surgical Intervention: May be necessary for treating ovarian cysts, fibroids, or endometriosis not responsive to medication.
When to Seek Medical Care
- Persistent or worsening pelvic pain
- Pain associated with fever, abnormal vaginal bleeding, or unusual discharge
- Unexplained or recurring pelvic discomfort
- Suspected pregnancy complications, such as pain during early pregnancy
When to Seek Immediate Medical Attention
- Severe, sudden-onset pelvic pain
- Suspected ectopic pregnancy
- Pelvic pain with high fever, chills, or heavy vaginal bleeding
- Signs of shock such as dizziness, fainting, or rapid heartbeat
Note: Some causes of pelvic pain, such as ectopic pregnancy or ovarian torsion, require emergency care. Always consult a healthcare provider for an accurate diagnosis and appropriate treatment plan.
Final Thoughts
Pelvic pain can stem from numerous causes, ranging from temporary discomfort to serious medical conditions. While occasional mild pain may resolve on its own, persistent or severe symptoms warrant medical evaluation. By understanding potential causes, from menstrual cramps and ovarian cysts to emergencies like ectopic pregnancy, you can make informed decisions about seeking care. Early diagnosis often leads to more effective treatment, so don’t hesitate to consult your healthcare provider if you experience concerning symptoms. With proper management, most pelvic pain can be improved, helping you regain comfort and quality of life.