If you’re experiencing pelvic pain, heavy periods, or other menstrual symptoms, you might be wondering whether adenomyosis or endometriosis could be the cause. These two conditions share similarities but affect the body in different ways. Understanding their differences can help you seek the right diagnosis and treatment.
In this article, we’ll explore how adenomyosis and endometriosis develop, their distinct symptoms, and how they impact daily life. We’ll also discuss diagnosis methods and treatment options to help you manage these conditions effectively.
What Are Adenomyosis and Endometriosis?
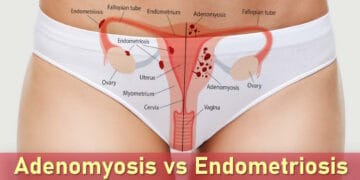
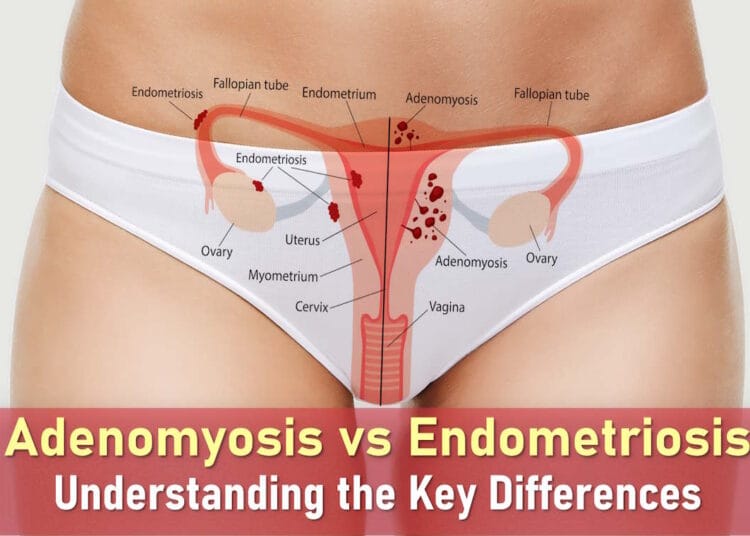
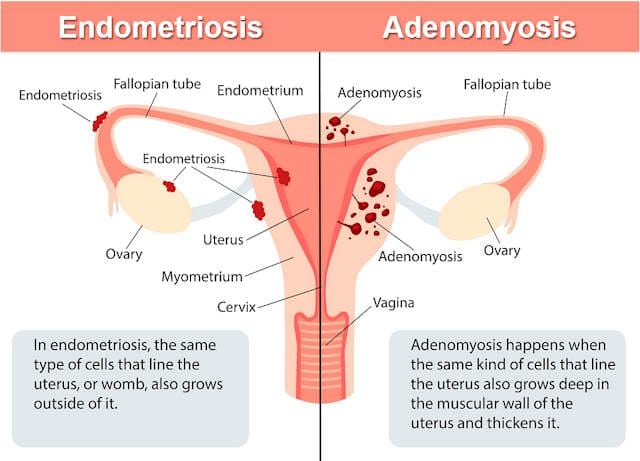
Adenomyosis and endometriosis both involve endometrial-like tissue growing where it shouldn’t, but their locations differ:
- Adenomyosis occurs when this tissue grows into the uterine muscle, making the uterus thicker and often causing heavy bleeding and severe cramping.
- Endometriosis happens when similar tissue grows outside the uterus, attaching to organs like the ovaries, fallopian tubes, or bladder, leading to widespread pelvic pain.
In adenomyosis, endometrial cells embed themselves in the uterine wall, causing inflammation and swelling. Each menstrual cycle, these cells react to hormones, leading to pain and heavy bleeding.
Endometriosis is more complex. One leading theory suggests that during menstruation, some blood flows backward into the pelvis, allowing endometrial cells to implant outside the uterus. However, since many women experience retrograde menstruation without developing endometriosis, other factors—like genetics or immune system issues, likely play a role.
How to Tell the Difference: Adenomyosis vs Endometriosis
Symptoms Unique to Adenomyosis
Adenomyosis primarily affects the uterus, leading to:
- Heavy, prolonged periods: Bleeding that lasts longer than a week and soaks through pads or tampons quickly.
- Severe menstrual cramps: Deep, throbbing pain in the pelvis, often worsening with age.
- Pain during sex: Discomfort due to an enlarged, tender uterus.
- Abdominal pressure: A constant feeling of bloating or fullness in the lower abdomen.
Symptoms Unique to Endometriosis
Endometriosis affects areas beyond the uterus, causing:
- Chronic pelvic pain: Discomfort that persists throughout the menstrual cycle, not just during periods.
- Painful bowel movements or urination: Especially during menstruation, due to tissue growth near the bladder or intestines.
- Digestive issues: Bloating, nausea, or diarrhea linked to menstrual cycles.
- Radiating pain: Discomfort that spreads to the lower back or legs.
While both conditions cause pain, endometriosis tends to affect a wider area of the body, whereas adenomyosis symptoms are more centralized in the uterus.
Adenomyosis vs Endometriosis: Overlapping Symptoms
Adenomyosis and endometriosis share several similar symptoms, which frequently leads to misdiagnosis. Both conditions can cause:
- Severe menstrual pain: Intense cramping that often requires pain medication or bed rest.
- Chronic pelvic pain: Discomfort that persists beyond menstrual periods.
- Fertility challenges: While endometriosis is more commonly associated with fertility issues, adenomyosis can also make implantation difficult due to uterine changes.
Because of these overlapping symptoms, many women go years without a proper diagnosis. Imaging tests like ultrasound or MRI can help distinguish between the two conditions, but an accurate diagnosis often requires a specialist familiar with both disorders.
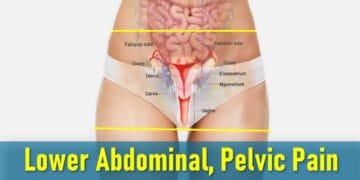
Adenomyosis vs Endometriosis Pain: Key Differences
Characteristics of Adenomyosis Pain
Women with adenomyosis typically experience:
- Deep, throbbing uterine pain: Often described as a constant, heavy pressure in the lower abdomen.
- Worsening during menstruation: Symptoms peak when the uterine walls become inflamed.
- Localized discomfort: Pain remains mostly centered in the uterus rather than spreading.
Many patients compare adenomyosis pain to extreme menstrual cramps that don’t fully subside between cycles.
Characteristics of Endometriosis Pain
Endometriosis pain differs in several ways:
- Widespread pelvic pain: Can radiate to the lower back, hips, and thighs.
- Sharp or stabbing sensations: Especially during bowel movements, urination, or intercourse.
- Unpredictable flare-ups: Unlike adenomyosis, pain may occur at any point in the menstrual cycle.
Because endometrial tissue can grow on multiple organs, the pain patterns tend to be more variable.
How Pain Affects Daily Life
Both conditions can significantly impact quality of life, but in different ways:
Living With Adenomyosis
Women with adenomyosis often:
- Plan work and social activities around their menstrual cycle
- Struggle with prolonged sitting or standing due to uterine pressure
- Experience fatigue from chronic pain and heavy bleeding
Living With Endometriosis
Endometriosis tends to create more unpredictable challenges:
- May need to cancel plans suddenly due to pain flare-ups
- Often limit physical activities to avoid triggering symptoms
- Deal with additional digestive or urinary symptoms
Both conditions can lead to emotional distress, especially when symptoms are dismissed or misunderstood by others.
Digestive Symptoms: Adenomyosis vs Endometriosis
How Adenomyosis Affects Digestion
While adenomyosis mainly impacts the uterus, it can cause:
- Bloating and abdominal pressure from an enlarged uterus
- Constipation due to uterine pressure on the rectum
- General abdominal discomfort, especially during periods
How Endometriosis Affects Digestion
Endometriosis often causes more direct digestive issues:
- Painful bowel movements if tissue grows near intestines
- Cyclical diarrhea or constipation
- Nausea and severe bloating (“endo belly”)
Treatment Approaches for Adenomyosis and Endometriosis
Heat Therapy
Applying a heating pad or warm compress to the lower abdomen can provide significant relief, especially for adenomyosis-related discomfort. The warmth helps relax uterine muscles and may ease digestive pressure caused by an enlarged uterus.
Medications and Supplements
Several options may help manage symptoms:
- Anti-inflammatory drugs: NSAIDs like ibuprofen can reduce pain and swelling
- Digestive support: Probiotics and enzymes may improve gut health and bloating
- Specialized supplements: Some women find relief with targeted nutrients, though professional guidance is recommended
Specialist Care
Consulting with a healthcare provider familiar with both conditions can help develop a personalized treatment plan, particularly for persistent digestive issues or severe pain.
When Both Conditions Occur Together
Research suggests about 20-30% of women with endometriosis may also have adenomyosis. When both conditions are present, symptoms often intensify, requiring comprehensive management strategies.
Lifestyle Management Tips
Symptom Tracking
Keeping a detailed record of:
- Pain levels and locations
- Menstrual cycle patterns
- Digestive symptoms
can help identify triggers and evaluate treatment effectiveness.
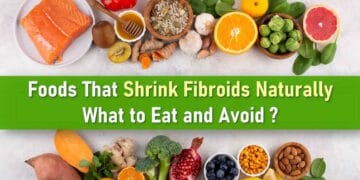
Anti-Inflammatory Approaches
Dietary changes that may help:
- Emphasizing fruits, vegetables, and omega-3 rich foods
- Reducing processed foods and added sugars
- Staying hydrated with water and herbal teas
Gentle Movement
Low-impact activities like:
- Walking
- Swimming
- Yoga or stretching
can improve circulation and reduce pelvic tension.
Stress Reduction
Mindfulness practices such as:
- Meditation
- Deep breathing exercises
- Therapeutic journaling
may help manage the emotional impact of chronic pain.
Medical Treatment Options
Hormonal Therapies
Common approaches include:
- Birth control pills to regulate cycles
- GnRH agonists to temporarily suppress hormones
- Progestin treatments to reduce tissue growth
Pain Management
Options may involve:
- Over-the-counter or prescription pain relievers
- Complementary therapies like acupuncture
- Specialized pain clinic approaches for severe cases
Surgical Options
When conservative treatments aren’t enough:
- Laparoscopy: Removes endometrial growths
- Adenomyomectomy: Targets adenomyosis tissue in the uterus
Supportive Therapies
Additional approaches that may help:
- Pelvic floor physical therapy
- Counseling or support groups
- Integrative medicine approaches
Adenomyosis and Fertility Considerations
Potential Impacts
Adenomyosis may affect fertility by:
- Altering the uterine environment for implantation
- Increasing risk of pregnancy complications
- Potentially contributing to miscarriage risk
Fertility Support Options
For women trying to conceive:
- Early consultation with a fertility specialist
- Hormonal treatments to improve uterine conditions
- Potential surgical options in select cases
With proper management, many women with adenomyosis can achieve successful pregnancies, though close monitoring is often recommended.
Long-Term Health Considerations and Treatment Options
Understanding Adenomyosis Long-Term Effects
While adenomyosis isn’t life-threatening, it can significantly impact quality of life and reproductive health. Potential long-term considerations include:
- Iron deficiency anemia: Chronic heavy bleeding may require iron supplements or dietary changes
- Fertility challenges: Uterine changes can affect implantation and pregnancy
- Pain management: Persistent discomfort may require ongoing treatment strategies
Many women experience symptom improvement during menopause as hormone levels change. However, for those still in their reproductive years, proactive management can help preserve fertility and overall wellbeing.
Surgical Options for Severe Cases
When conservative treatments aren’t effective, surgical approaches may be considered:
- Adenomyomectomy: Removes affected uterine tissue while preserving fertility
- Hysterectomy: Complete uterus removal for women not planning pregnancy
Regular follow-ups with a healthcare provider can help monitor symptoms and adjust treatment plans as needed.
Treatment Approaches for Both Conditions
Hormonal and Medication Therapies
Common first-line treatments include:
Hormonal Options
- Birth control methods: Pills, patches, or hormonal IUDs to regulate cycles
- GnRH medications: Temporarily reduce estrogen to shrink abnormal tissue
- Progestin therapy: Helps control tissue growth with fewer side effects
Pain Management Medications
- NSAIDs for inflammation and pain relief
- Prescription pain relievers for severe cases
Surgical Treatments: Key Differences
Endometriosis Excision Surgery
This minimally invasive procedure:
- Removes endometrial-like tissue from pelvic organs
- Can improve fertility outcomes
- Typically performed laparoscopically
Adenomyomectomy
This uterine-preserving surgery:
- Targets affected areas within the uterine wall
- Requires extended recovery before attempting pregnancy
- May provide significant symptom relief
Hysterectomy remains an option for women with severe symptoms who have completed childbearing.
Comprehensive Pain Management Strategies
Supportive Therapies
Additional approaches that can complement medical treatment:
- Pelvic floor therapy: Specialized physical therapy to relieve muscle tension
- Acupuncture: May help reduce pain for some patients
- Nerve blocks: Temporary pain relief for severe cases
Lifestyle Modifications
Daily habits that may improve symptoms:
Dietary Changes
- Anti-inflammatory foods (leafy greens, berries, fatty fish)
- Reducing processed foods and added sugars
- Adequate hydration
Movement and Stress Relief
- Gentle exercise like walking or swimming
- Yoga for flexibility and relaxation
- Mindfulness practices to manage stress
Creating a Personalized Treatment Plan
The most effective approach often combines multiple strategies:
- Medical treatments tailored to symptom severity
- Surgical options when appropriate
- Supportive therapies for daily management
- Lifestyle adjustments to support overall health
Working with a healthcare team including gynecologists, pain specialists, and physical therapists can help create a comprehensive plan addressing all aspects of these conditions.
Stages of Adenomyosis and Endometriosis
Adenomyosis Severity Levels
While adenomyosis doesn’t have formal stages like endometriosis, healthcare providers often describe its progression in terms of severity:
- Mild adenomyosis: Tissue is found in the outer uterine muscle layer, typically causing occasional cramps and moderate bleeding
- Moderate adenomyosis: Deeper muscle involvement leads to heavier periods and more frequent pelvic discomfort
- Severe adenomyosis: Widespread muscle involvement causes intense symptoms including chronic pain and significant uterine enlargement
- Diffuse adenomyosis: Affects nearly the entire uterine wall, often resulting in the most severe symptoms and potential fertility impacts
This classification helps guide treatment decisions, from medication management to surgical options.
Endometriosis Staging System
The American Society of Reproductive Medicine classifies endometriosis into four official stages:
- Stage 1 (Minimal): Few shallow implants with little to no scarring
- Stage 2 (Mild): More widespread but still relatively shallow implants
- Stage 3 (Moderate): Deeper implants with more noticeable scarring and possible ovarian involvement
- Stage 4 (Severe): Extensive deep implants affecting multiple organs with significant scarring
This staging system helps determine appropriate treatment approaches and provides insight into potential fertility impacts.
Daily Management Strategies
Pain and Fatigue Management Techniques
Living with both conditions requires practical approaches to manage symptoms:
Energy Conservation
- Pace activities throughout the day
- Schedule regular rest periods
- Prioritize essential tasks
Pain Relief Methods
- Heat therapy (heating pads, warm baths)
- Gentle stretching and movement
- Over-the-counter or prescription pain medication as needed
Movement and Exercise
- Low-impact activities like swimming or walking
- Yoga for flexibility and relaxation
- Listening to your body’s limits
Nutritional Support
- Anti-inflammatory foods (berries, leafy greens, fatty fish)
- Adequate hydration
- Reducing processed foods and caffeine
Conclusion: Taking Control of Your Health
While adenomyosis and endometriosis can significantly impact quality of life, understanding these conditions empowers you to seek appropriate care. Key takeaways include:
- Both conditions have distinct characteristics but may occur together
- Various treatment options exist, from medication to surgical approaches
- Lifestyle modifications can complement medical treatments
- Professional guidance helps create personalized management plans
With proper management strategies, many women find effective ways to reduce symptoms and maintain active, fulfilling lives. If you suspect you have either condition, consult a healthcare provider specializing in these disorders for accurate diagnosis and tailored treatment options.